当前位置:AASLD-美国肝病研究学会年会 » 正文
巅峰对话丨代谢相关脂肪性肝病:话诊疗新进展,议新加坡和美国经验,遏制全球化进程
—— 作者: 时间:2023-12-27 10:37:02 阅读数:
36

编者按
非酒精性脂肪性肝病(NAFLD)/代谢相关脂肪性肝病(MASLD)在全球范围内呈逐步上升流行趋势,目前已发展成为我国慢性肝脏疾病的首要病因,对人民健康构成重大威胁。围绕危险因素建立诊断模型协助临床进行诊断分级,或研发无创评估手段,是发现更多患者并有效干预疾病进程的重要前提。
新加坡国立大学医院助理教授Daniel Q Huang在NAFLD/MASLD领域有颇多建树,他在2023年美国肝病研究学会年会(AASLD2023)上交流了团队诸多相关研究新进展。美国西达赛奈医学中心消化科杨毅辉(Yee Hui Yeo)博士在该领域亦有诸多探索和发现。《国际肝病》特邀两位青年专家就NAFLD/MASLD筛查诊断、新药研发等热点问题进行对话,相关内容分享如下。

01
NAFLD家族风险评分,一种切实可行的筛查策略
《国际肝病》
本届美国肝病研究学会年会上,您介绍了团队开发的NAFLD家族风险评分的最新研究进展[1],能否请您谈谈主要研究结果及其重要意义?
Daniel Q Huang
非酒精性脂肪性肝病(NAFLD)相关纤维化具有遗传性,但尚不清楚如何利用家族史来鉴定进展期纤维化的一级亲属。我们旨在开发和验证一种简单的风险评分,以确定接受了肝纤维化评估的先证者的一级亲属中有较高NAFLD合并进展期纤维化风险者。
为了获得这个评分,我们纳入了两个前瞻性队列(来自美国圣地亚哥的派生队列和来自芬兰赫尔辛基的验证队列)。我们通过MRI或弹性成像评估所有受试者的肝纤维化状态,确定与进展期纤维化相关的关键因素。
重要的是,在这项评分中,我们发现家族史是一级亲属进展期纤维化风险的主要组成部分。因此,我们设计了一个简易的评分,包括年龄(≥50岁)、2型糖尿病、肥胖和家族史,我们希望可以轻松地发现那些有进展期肝纤维化高风险的一级亲属(图1)。
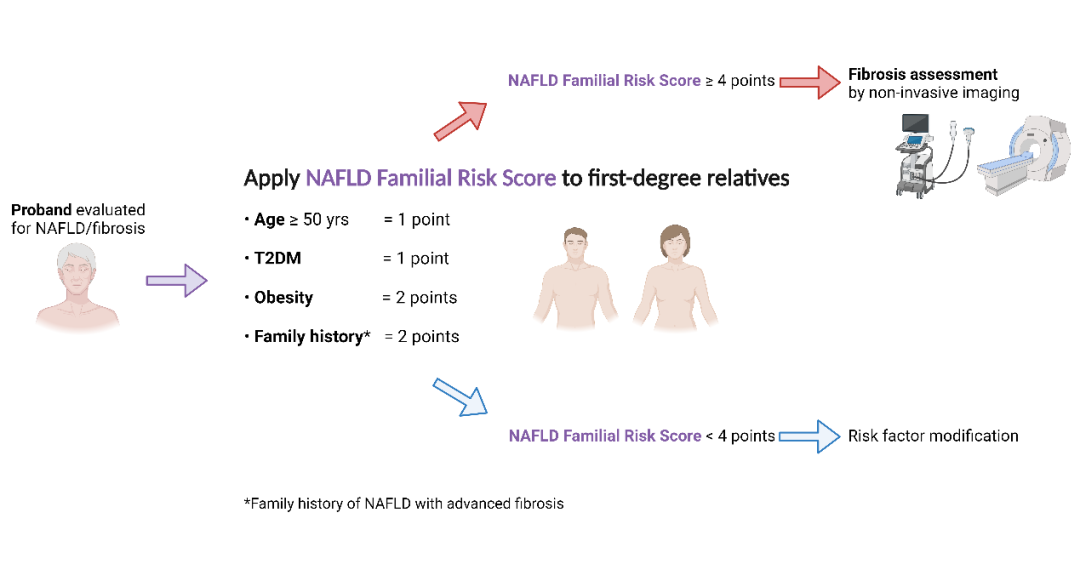
图1. NAFLD家族风险评分[1]
杨毅辉(Yee Hui Yeo)
我想强调的是,这个家族风险评分真的很重要,建立得非常及时。根据我们此前的分析,2020年的NAFLD/MASLD总体流行率已达到约39%,预计至2040年,NAFLD/MASLD流行率将逼近55%。很多预测模型均提示,仍有大量进展期肝纤维化病例未被发现,而NAFLD家族风险评分将有助于识别那些未确诊的患者。
此外,特别值得关注的是,这是一种相对可行、可操作的方法,可以简便地识别或捕获足够多的未确诊患者,因为他们是从家庭成员那里获得转诊。毫无疑问,这是一种切实可行的策略。
英文原文:
<Hepatology Digest>: At the annual meeting of the American Association for the Study of Liver Disease, you introduced the latest research progress of the NAFLD Familial Risk Score developed by your team. Could you please talk about the main research results and its significance?
Daniel Q Huang: Nonalcoholic fatty liver disease (NAFLD)-related fibrosis is heritable, but it is unclear how family history may be used to identify first-degree relatives with advanced fibrosis. We aimed to develop and validate a simple risk score to identify first-degree relatives of probands who have undergone assessment of liver fibrosis who are at higher risk of NAFLD with fibrosis.
To develop this score, what we did was we leverage on two prospective unique formula cohorts (derivation, validation). We assess liver fibrosis status in all participants by either MRI or elastography. We identify key factors that were associated with advanced fibrosis.
Importantly, in this score, we found that family history is a major component of the risk of advanced fibrosis in first-degree relatives. So, we devised a very simple score comprising of age, diabetes status, obesity, and family history that we hope can easily identify first-degree relatives of people who already are going to have advanced fibrosis that are higher risk themselves.
Yee Hui Yeo: I would like to emphasize that this family score is really important and the finding is timely. The main reason is that our previous analysis shows that the overall prevalence of MASLD currently, even in 2020, the modeling shows that it's almost 39% and is forecast to be almost 55% in 2040. And there are just so many undiagnosed cases around with more scores like this. It will help to identify those who are undiagnosed.
This is a relatively feasible, actionable way to identify or capture patients with undiagnosed MASLD, given that they got this referral from family members. Definitely, this is a pragmatic way for us to practice as a political provider.
02
开展常规风险分层,血液指标结合影像评估
《国际肝病》
亚洲代谢相关脂肪性肝病患者人数逐年上升,迫切需要更为有效的无创诊断手段用于临床。从科学研究的角度,您怎么看无创诊断的机遇和挑战?较具前景的研究方向?
Daniel Q Huang
代谢相关脂肪性肝病的无创诊断是一个未满足需求的巨大领域。我认为,在过去的一两年中,AASLD和AGA已经为我们如何对这些患者进行风险分层提供了指导,尤其是那些有代谢危险因素的患者。
我认为在亚洲,我们确实需要通过从四大指标开始,然后通过进一步影像学评估来分层。我认为,尽管这是一个仍需要我们改进的领域,因为现有策略有较多缺陷,但目标人群未来应常规进行分层。
我们小组正在研究基于MRI的策略。但与此同时,我们也担心这种策略可能不会广泛适用于普通人群。因此,我认为其他基于血液的生物标志物是关键和必不可少的。这是一个我们希望在未来一两年内有望取得更多成果的领域。
杨毅辉(Yee Hui Yeo)
非常同意黄教授所说,同时,在亚洲,MAFLD的一些生物标志并非常规检测项目。因此,我们需要考虑一些更容易执行的策略,并帮助提高准确性,特别是当涉及亚洲大众或亚洲患者时,毕竟亚洲人群里正常或低BMI的脂肪肝患者很多。
此外,我们需要考虑伴随着各种感染背景下的NAFLD/MASLD流行情况。例如,新版AASLD脂肪变性肝病指南将这种情况下的所有肝炎病毒感染均归纳到MASLD定义中。然而,我们不知道这些已有影像学证实的脂肪变性患者中,肝炎病毒感染与代谢综合征之间的相互作用。未来在使用无创检测诊断NAFLD/MASLD方面有更多潜在研究方向。我们期待黄教授在这方面的更多发现。
英文原文:
<Hepatology Digest>: The number of patients with metabolic dysfunction-associated fatty liver disease in Asia is increasing year by year, and more effective noninvasive diagnostic methods are urgently needed for clinical use. From the perspective of scientific research, how do you see the opportunities and challenges of noninvasive diagnosis? More promising research directions?
Daniel Q Huang: That's a great area of unmet need. I think, in the last 1 or 2 years, the AASLD and the AGA have provided guidance in terms of how we might risk stratify such patients, but especially those with metabolic risk factors.
I think in Asia, we do need to validate these pathways specifically by starting with big four and then stratifying further by last pathography. I think though this is an area that we still need improvement on, because there are many drawbacks of such approaches, there will be participant patients that are classified routinely. Those advanced versus might have a little bit for or vice versa. So, I think this is an area of unmet need.
Our group is working on MRI based strategies. But at the same time, we are also concerned that such strategies may not be widely available for the general population. So I think other blood based biomarkers are key and essential. And this is an area that we hope to have more results in the next 1 or 2 years.
Yee Hui Yeo:
I really want to second what Doctor Huang just mentioned about the usability and some of the challenges that we have. Currently, some of the biomarkers of MAFLD are not routinely tested. So, we need to think about some of the more accessible strategies and also to help to increase the accuracy, especially when it comes to Asian audiences or Asian patients.
Then we need to think about the prevalence when, in the background, there are a lot of people with a concomitant variety of infections. In that case, for example, for the most recent AASLD guideline of steatotic liver disease, viral hepatitis infections are included in that definition. However, we do not clearly know what their roles are or the interplay between the virus infection and the existence of metabolic syndrome among all these patients with imaging-proven steatotic liver disease.
There is future potential for more research in terms of using the noninvasive test to diagnose MASLD. And we're looking forward more work from Dr Huang really.
03
糖尿病影响NAFLD/MASLD进展,控制血糖是干预重点
《国际肝病》
您认为哪些因素可以预测代谢相关脂肪性肝病的进展?
Daniel Q Huang
我认为进展的一个主要决定因素是是否存在2型糖尿病(T2DM)。在我们最近的一项工作中,我们发现,相比无T2DM者,T2DM患者的纤维化进展速度明显更快(图2)[2]。此外,我们还发现,相比糖化血红蛋白(HbA1c)较低的受试者,HbA1c较高者与肝硬化进展更快显著相关[3]。因此,我认为,尽管纤维化进展有许多决定因素,包括遗传、HbA1c、糖尿病等,但总体而言,血糖控制无疑是需要关注的一个主要领域。
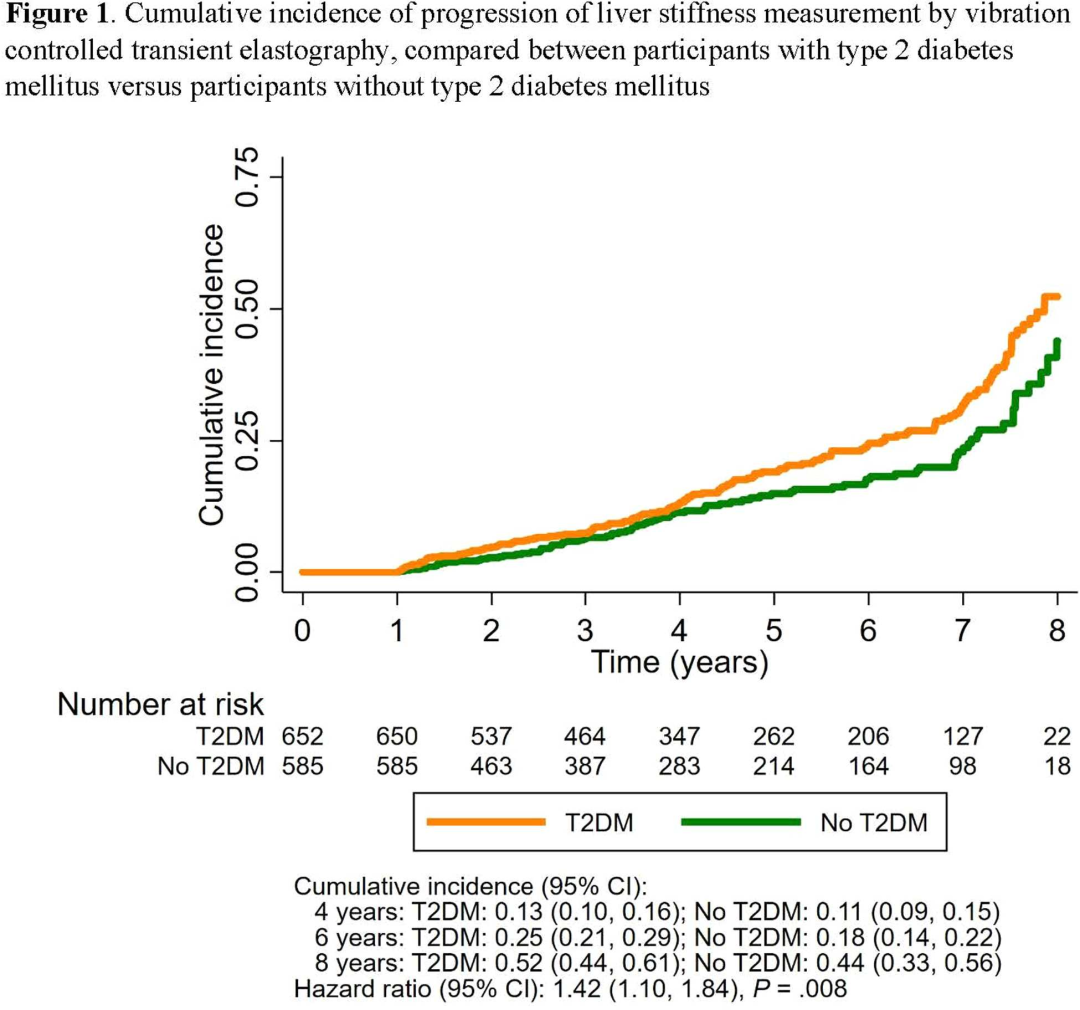
图2. T2DM与无T2DM者的累积LSM进展比较[2]
杨毅辉(Yee Hui Yeo)
完全同意。这确实是一项重要的研究,使用连续活检来证实糖尿病人群里疾病机制和NAFLD/MASLD的存在。在亚洲患者中,代谢综合征、肝炎病毒感染和酒精的使用等共病症可以加重病情的恶化,同时,我们如何去发现风险因素并剖析其对疾病恶化的作用是非常重要的。举例,我们应更加关注可修正的风险因素,例如HbA1c、代谢综合征、营养管理和体能锻炼都很重要。
英文原文:
<Hepatology Digest>: What factors do you think can predict the progression of metabolic dysfunction-associated fatty liver disease?
Daniel Q Huang: Great question. If we, so I think one major determinant of progression is the presence of type two diabetes. In one of our recent works, we have shown that among patients with type two diabetes, these patients have a significantly faster progression rate of fibrosis compared to those without T2DM.
And in a poster that we presented yesterday, we also found that a higher HbA1c is significantly associated with faster progression of liver stiffness compared to participants with a lower HbA1c. So, I think while there are many determinants of fibrosis progression, including genetics, HbA1c, diabetes, and glycemic control is certainly one major area to focus on.
Yee Hui Yeo: Fully agree. That is an important study that used a sequential biopsy to prove the mechanism of disease and the existence of a true NAFLD among patients with diabetes. I think back in Asian patients, we have metabolic syndrome, hepatitis infection and alcohol-related liver disease. How we decipher the role of some other risk factors and how they can predict the progression is important. For example, I would focus more on the modifiable risk factor, say, HbA1c, the control of a metabolic syndrome, nutrition, and physical exercise will be important.
04
减重和调整饮食,可带来长远获益
《国际肝病》
您怎么评价这些可改变或调整的风险因素?
Daniel Q Huang
我们有这么多可改变的风险因素,其中一个重要的决定因素实际是坚持行动和等待改变。我认为,受试者或患者只要获得了体重减轻,不一定需要达到体重的10%,因为这对于大多数患者而言是无法实现的,即使是减重1~2kg,从长远来看,也会发挥积极作用。除此之外,我认为改变患者的饮食也非常重要,尤其是减少含糖量高的饮料和食物摄入是有必要的。
杨毅辉(Yee Hui Yeo)
谈及体重,有几种较熟悉的用于控制体重的药物,例如司美格鲁肽(Semaglutide)等GLP-1受体激动剂都对控制NAFLD/MASLD、NASH/MASH有很大潜力。
英文原文:
<Hepatology Digest>: What's your comment on this modifiable risk factor?
Daniel Q Huang: Great question. If I think there are so many modifiable risk factors, I think one important determinant actually will be wait. I think if participants or patients are able to lose weight, it doesn't necessarily need to be 10 % of the body weight, because that is unachievable for most of our patients. But even one kg 2 kilograms any bit, I think I feel helps in the long run. And beyond that, I think modifying our diet of our patients is also really important, especially cutting down in terms of high fructose containing drinks and foods essential.
Yee Hui Yeo: Right. Speaking about weight, there are several well-known medications that are approved for weight control, like semaglutide and liraglutide (GLP-1 receptor agonists), are found to have potential to control NAFLD, MASLD, NASH/MASH.
05
NAFLD/MASLD新药,黎明前的曙光
《国际肝病》
您怎么评价这些药物的未来前景?
Daniel Q Huang
我认为这是令人激动的时刻。虽然目前这些新药(例如GLP-1受体抑制剂)尚未获批用于NASH治疗,但在2型糖尿病、肥胖症和NASH患者,我们看到越来越多的证据表明这些新药物可能对自然消退或进展期纤维化逆转有用。
因此,我真的很希望随着更多的试验公布,我们有更多的数据表明,至少其中一些药物会被批准。我认为在这个时候,可能更多是等待和观察,但我对不久的将来充满希望。
杨毅辉(Yee Hui Yeo)
确实,这些药物已经用于治疗糖尿病很长一段时间了,希望未来能够获得FDA批准。
英文原文:
<Hepatology Digest>: What's the potential for these medications?
Daniel Q Huang: I think these are exciting times inward. At this point time, these new medications, such as GLP-1 against, they have not been specifically approved for NASH, but in our patients with type 2 diabetes or obesity and who have NASH at the same time, I think we are increasingly seeing more and more evidence that these new agents may be useful for natural resolution or advanced fibrosis regression.
So, I'm really hopeful that as more of the trials come out, and we have more data that at least some of these medications will be approved. I think at this point in time, it's probably more of a wait and see approach, but I’m hopeful for the near future.
Yee Hui Yeo: for sure. Yeah, again, these are medications that have been used for diabetes for quite a long time. And hopefully, this can help with, again, the accessibility of the medication in the future when it is approved by the FDA.
06
多学科协作,从NAFLD/MASLD知识普及和筛查开始
《国际肝病》
在代谢相关脂肪性肝病的临床治疗和管理方面,新加坡是否有一些比较有效的策略?仍有哪些待解决问题?
Daniel Q Huang
NAFLD/MASLD在新加坡当然是一个大问题,与亚洲其他地区一样。事实上,在过去的十年中,我们已经看到了乙型肝炎的巨大改变,现在更为重要的是NAFLD/MASLD,我们的移植门诊现在挤满了NAFLD/MASLD相关HCC患者。我认为我们必须逐一解决一些重大问题。其中之一就是新加坡民众对NAFLD/MASLD的总体认识不足。因此,我认为要对普通大众和公共卫生提供者进行相关知识普及。
此外,我们需要与其他专业的合作伙伴,例如公共卫生提供者、内分泌学专家,进行更为密切的合作,例如,开展NAFLD/MASLD筛查是重要的措施。AASLD和AGA修订的指南为此提供了很好的参考,但我们需要将AASLD或AGA的各种建议调整为适用于东南亚当地人群的指导意见。
杨毅辉(Yee Hui Yeo)
非常赞成黄教授的观点,多学科协作很重要。回到美国,也是如此。我们仍有许多人未被诊断,并且,一些初步数据显示,那些首次诊断出NAFLD/MASLD相关肝硬化或NAFLD/MASLD相关HCC的患者中,很多已经处于失代偿期肝硬化状态。不同于慢性肝炎和饮酒所致酒精性肝病的患者,大众对代谢综合征对肝脏的危害尚没有充分的了解,因此我们必须真正提高大众的相关认知。
英文原文:
<Hepatology Digest>: Is there any effective strategy for the clinical treatment and management of MASLD in Singapore? And any other challenge of problems remained to be resolved?
Daniel Q Huang: Great question. MASLD is certainly a big problem in Singapore and same as the rest of Asia. In fact, in the last decade, we have seen a huge swing away from hepatitis B, do what's more MASLD, our transplant clinics are full of patients now with MASLD and HCC. And I think there are major issues that we have to tackle one by one. One of them actually is a poor awareness of MASLD in general in Singapore.
I think a lot of education is to be done both to the general population as well as have health care providers. We need to work more closely with our partners from other specialties, public health officials, endocrinologist. I think one area that we can potentially look into doing is implementing some form of screening for MASLD. I think the AASLD and AGA revised guidelines, guidance is a useful starting point. But we do need to tailor these cut points and the various guidance from AASLD or AGA to our local population in southeast Asia.
Yee Hui Yeo: Definitely. Totally appreciate your points in terms of recalibrating the cut-off for this test. And also, it's important as well for the multidisciplinary care of these patients. And back in the United States, we face a similar situation. There are still a lot of people being undiagnosed and also from some preliminary data, the first time when MASLD-related cirrhosis or MASLD-related HCC are diagnosed, the patients already show decompensated cirrhosis.
So, unlike the patients with viral hepatitis, who are being followed for a long time, or at least patients who are aware of a liver disease such as those with alcohol-related disease, patients with MASLD are more unlikely to be aware of their disease status. Thus, we must promote the awareness of the risk of metabolic syndrome towards liver health.
07
NAFLD/MASLD防控的拐点,迫切需要改变
《国际肝病》
您是否还有其他补充意见?
Daniel Q Huang
完全同意您提出的重要问题。我认为NAFLD/MASLD现在是个大问题。而且,我认为亚洲各国都面临着这个问题。因此,我认为我们确实需要加强国家之间以及各国内部的合作,才能真正解决这个问题。我认为我们正处于一个转折点,如果我们不利用这段时间有效地教育我们的民众,并制定全国性的战略来应对NAFLD/MASLD,我们将承受后续的严重后果。因此,我认为这是一个非常需要和紧迫的领域。
杨毅辉(Yee Hui Yeo)
完全同意。我希望我们此前建立的对2040年疾病流行的预测模型能够因为NAFLD/MASLD被有效控制而被逆转/推翻。
英文原文:
<Hepatology Digest>: Are there any other last comments to this session?
Daniel Q Huang: All right. I fully agree with the important issues that you raise. I think MASLD is now such a large problem. And it's, I think the various countries in Asia are facing it. So, I think we really need stronger collaboration above between countries and within each country to really tackle this problem. I think we are at the cusp of like a turning point where, if we do not use this time to effectively educate our population and institute nationwide strategies to tackle NAFLD, we will suffer the consequences downstream. So, I think this is an area of great need and urgency.
Yee Hui Yeo: Fully agree. I hope that the forecast modeling that we made for 2040 can be overturned so that it won't happen in the future.
参考文献:
[1] Huang DQ, Ahlholm N, Luukkonen P, et al. Development and validation of the NAFLD familial risk score to detect advanced fibrosis: a prospective, multicenter study. AASLD 2023. Oral 236.
[2] Huang DQ, Wilson L, Amangurbanova M, et al. Liver stiffness progression in biopsy-proven nonalcoholic fatty liver disease among people with diabetes versus people without diabetes: a multicenter study. AASLD 2023. Poster 2067-A.
[3] Tamaki N, Wakabayashi S, Kimura T, et al. Glycemic control target associated with a lower risk of liver-related and cardiovascular events in nonalcoholic fatty liver disease. AASLD 2023. Poster 2182-A.
专家简介

Daniel Q Huang
新加坡国立大学医院助理教授,主要研究领域包括肝细胞癌、非酒精性脂肪性肝病、乙型肝炎和肝硬化等。2022年荣获美国肝病研究学会基金会奖。以第一和通讯作者发表同行评议文章105篇,其中有13篇影响因子>20,H-Index为16。

杨毅辉
美国洛杉矶Cedars-Sinai(西达赛奈)医院消化科在训。毕业于中国台湾国防医学院、牛津大学,博士后研究师从斯坦福大学Mindie Nguyen教授。专注于肝病领域的流行病学、临床医学以及机器学习的研究。2019年获美国肝病学会颁Emerging Liver Scholar。以第一和通讯作者发表在JAMA Oncology、Journal of Hepatology、Gastroenterology、Gut、Hepatology、AJG等100篇文章,引用4204次。

声明:本文仅供医疗卫生专业人士了解最新医药资讯参考使用,不代表本平台观点。该信息不能以任何方式取代专业的医疗指导,也不应被视为诊疗建议,如果该信息被用于资讯以外的目的,本站及作者不承担相关责任。
标签:
访谈
巅峰对话
其他肝病
发表评论
全部评论