JOH丨TIPS术后肝性脑病是否增加肝硬化患者的死亡率?
—— 作者: 时间:2024-07-01
阅读数:
22
编者按:近日,意大利学者Silvia Nardelli教授等一项发表在Journal of Hepatology杂志上的研究发现,肝硬化患者在接受经颈静脉肝内门体分流术(TIPS)后,即使发生显性肝性脑病(OHE),其死亡率并未显著增加。这一结论颠覆了既往人们对非TIPS背景下OHE负面影响的认识,为肝硬化患者提供了新的治疗希望和管理策略。
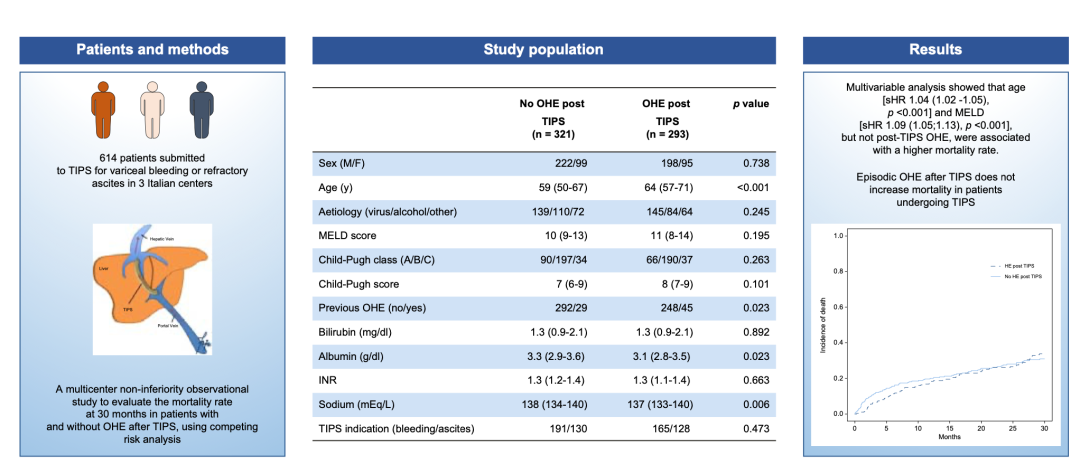
图1. 文章重要图表摘要
(https://doi.org/10.1016/j.jhep.2023.11.033)
经颈静脉肝内门体分流术(TIPS)是一种越来越广泛使用的非手术放射学介入治疗门脉高压并发症的方法。TIPS在门静脉和肝静脉之间建立连通,将血流直接从门静脉循环转移到全身血管床,通过降低门体压力梯度有效地减压门静脉系统。自20世纪80年代末推出以来,TIPS已成为门脉高压并发症患者的一种既定治疗方法,主要用于治疗静脉曲张再出血和复发性或难治性腹水[1-3]。在这些情况下,TIPS被证明可以提高患者的生存率,但研究表明存在一些差异[4-9]。
显性肝性脑病(OHE)是TIPS置入术后与分流相关的主要并发症。据报道,肝硬化患者TIPS术后OHE的发生率在术后第一年内高达35%-50%,接受TIPS治疗的患者中高达8%可能会出现持续性OHE[10-14],在选定的病例中,需要通过减少支架直径来控制[14,15]。这些发现促使了许多研究,旨在确定TIPS后OHE发展的风险因素,以改善患者的选择,以及探索预防TIPS术前OHE的药理学策略的研究。年龄较大、终末期肝病(MELD)或Child-Pugh评分较高、既往有明显或轻微HE病史、少肌症、肾功能受损、大分流直径和较低的衍生后门体压力梯度已被证明会增加发生TIPS后OHE的可能性[14,16-22]。因此,现有指南鼓励尽可能根据上述报告的因素选择TIPS患者[1-3]。预防TIPS后OHE的药物管理仍存在争议[23,24]。
在TIPS之外的肝硬化患者中,无论肝硬化的严重程度或是否存在急性或慢性肝功能衰竭,OHE的发展都会对生存产生不良影响[25]。在等待肝移植(LT)的患者中,至少发生一次OHE会增加6个月的死亡率,并显著提高MELD评分的预测值[26]。然而,在TIPS后发展为OHE的患者中是否也观察到死亡率增加,尚未具体解决。现有的几种评分,如Child-Pugh评分、MELD评分、FIPS(TIPS后生存的弗赖堡指数)评分和最近发表的ExPeCT评分,有助于确定TIPS后预后不良的高风险患者[27-30]。然而,这些评分并不认为TIPS后OHE是影响生存的潜在因素,并且尚未在大量人群中研究TIPS后OHE对死亡率的影响[31]。TIPS后OHE的发生是否会增加TIPS患者的死亡率仍不确定。
鉴于此,意大利学者Silvia Nardelli教授等设计了一项多中心、非劣效性的观察性研究[32],以比较根据TIPS后OHE发生率划分的TIPS患者的死亡率。该研究由意大利多家医疗中心联合开展,对614名接受TIPS治疗的肝硬化患者进行了长达30个月的跟踪观察。结果显示,尽管47%的患者在术后出现了至少一次OHE,但多因素分析表明,年龄和MELD评分才是影响死亡率的独立因素,而OHE并未增加患者的死亡风险。这一发现打破了传统观念,即在非TIPS治疗的肝硬化患者中,OHE常被视为预后不良的强烈指标。
然而,该研究团队同时也指出,TIPS术后患者可能经历了更严格的筛选和更密切的监测,这可能是导致OHE不增加死亡率的原因之一。此外,虽然阵发性OHE不增加死亡率,但其对患者生活质量和发病率的影响仍不容忽视,特别是持续性OHE患者,其死亡率显著高于未发生OHE的患者。
这项研究不仅为肝硬化患者的管理提供了重要依据,还强调了个性化治疗和患者选择的重要性。研究人员建议,对于潜在的高风险患者,应采取更严格的术前评估、术中操作及术后管理策略,以减少OHE的发生,并特别关注持续性OHE的预防和治疗。
在此之后,奥地利维也纳大学Lukas Hartl教授基于这篇文章的成果,进一步分析和探讨了TIPS后早期出现脑病是否影响患者的死亡率[33]。他们通过回顾性研究,分析了维也纳2000年9月至2022年11月间接受TIPS治疗的237名患者,排除了具有血管性肝病、肝细胞癌、先前肝移植或预防性TIPS植入的患者。主要终点是30个月死亡率,并设置了1、3和6个月后的里程碑来分析OHE对死亡率的影响。
结果发现,在TIPS后3个月和6个月出现OHE的患者在死亡率方面并未显示出显著差异,支持了Silvia Nardelli教授的研究结果。然而,该项研究发现在TIPS后1个月即出现OHE的患者显示出了显著更高的死亡率。累积发病率分析显示,这些患者1年和2年的死亡率分别为43.6%和48.1%,而未出现OHE的患者分别为13.9%和20.2%(P=0.004,图2)。
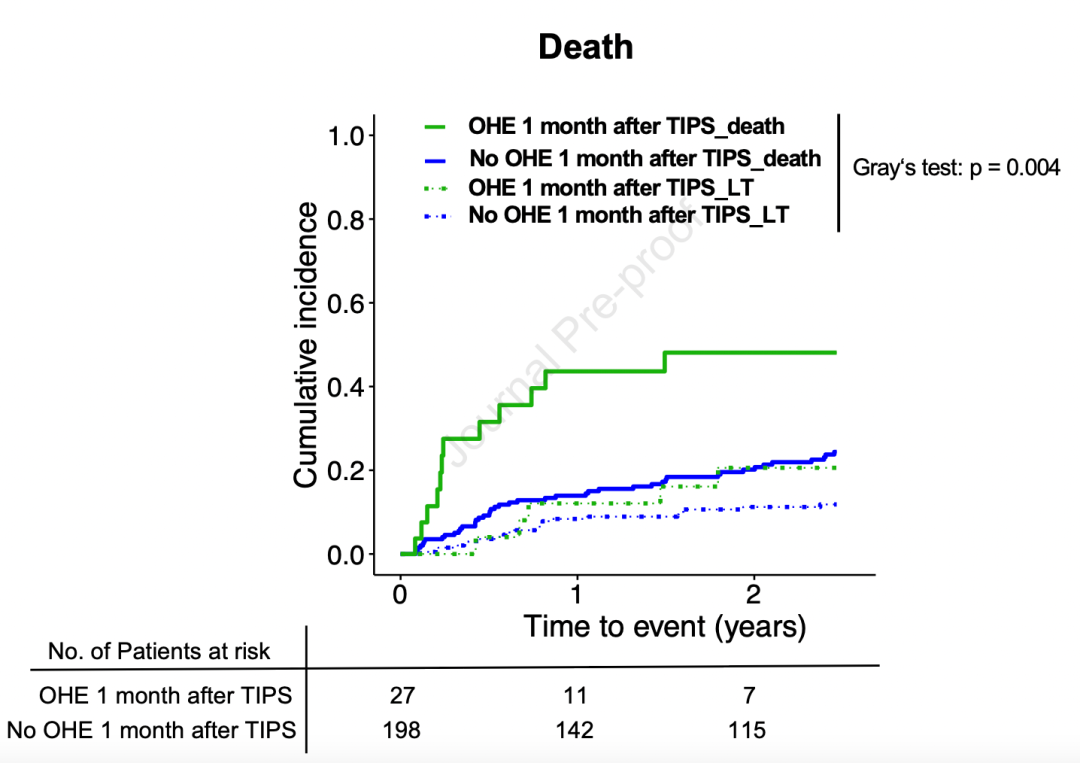
图2. TIPS后1个月即出现OHE的患者的累积发病率
(https://doi.org/10.1016/j.jhep.2024.05.035)
尽管TIPS后3个月和6个月出现的OHE对死亡率无显著影响,但早期(1个月内)出现的OHE与显著增加的死亡率相关。这表明早期出现OHE的患者可能面临更高的死亡风险,值得进一步研究和关注。
Lukas Hartl教授的这项研究为理解TIPS后OHE对死亡率的影响提供了新的见解,并强调了早期识别和干预OHE的重要性。同时,该研究结果也提醒医生在TIPS术后应密切监测患者,以便及时发现并处理OHE。
综上所述,当前基于TIPS后OHE对死亡率影响的研究成果对于改善肝硬化患者的预后、提高生活质量具有重要意义,也为未来的临床研究和治疗提供了新的方向。随着研究的深入,我们有理由相信,更多有效的管理和治疗策略将被发现,为肝硬化患者带来更好的健康前景。
参考文献:
[1] de Franchis R, Bosch J, Garcia-Tsao G, et al. Baveno VII - renewing consensus in portal hypertension. J Hepatol 2022 Apr;76(4):959–974.
[2] Fagiuoli S, Bruno R, Debernardi Venon W, et al. AISF TIPS Special Conference. Consensus conference on TIPS management: techniques, indications, contraindications. Dig Liver Dis 2017 Feb;49(2):121–137.
[3] Tripathi D, Stanley AJ, Hayes PC, et al. Transjugular intrahepatic portosystemic stent-shunt in the management of portal hypertension. Gut 2020 Jul;69(7):1173–1192.
[4] Nicoara-Farcau O, Han G, Rudler M, et al. Preemptive TIPS individual data metanalysis, international variceal bleeding study and baveno cooperation study groups. Effects of early placement of transjugular portosystemic shunts in patients with high-risk acute variceal bleeding: a meta-analysis of individual patient data. Gastroenterology 2021 Jan;160(1):193–205.e10.
[5] Salerno F, Cammà C, Enea M, et al. Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Gastroenterology 2007 Sep;133(3):825–834.
[6] Bureau C, Thabut D, Oberti F, et al. Transjugular intrahepatic portosystemic shunts with covered stents increase transplant-free survival of patients with cirrhosis and recurrent ascites. Gastroenterology 2017 Jan;152(1):157–163.
[7] Narahara Y, Kanazawa H, Fukuda T, et al. Transjugular intrahepatic portosystemic shunt versus paracentesis plus albumin in patients with refractory ascites who have good hepatic and renal function: a prospective randomized trial. J Gastroenterol 2011 Jan;46(1):78–85.
[8] Deltenre P, Zanetto A, Saltini D, et al. The role of transjugular intrahepatic portosystemic shunt in patients with cirrhosis and ascites: recent evolution and open questions. Hepatology 2023 Feb 1;77(2):640–658.
[9] Larrue H, D’Amico G, Olivas P, et al. TIPS prevents further decompensation and improves survival in patients with cirrhosis and portal hypertension in an individual patient data meta-analysis. J Hepatol 2023 May 2;S0168-S8278(23):314–318.
[10] Riggio O, Merli M, Pedretti G, et al. Hepatic encephalopathy after transjugular intrahepatic portosystemic shunt. Incidence and risk factors. Dig Dis Sci 1996 Mar;41(3):578–584.
[11] Somberg KA, Riegler JL, LaBerge JM, et al. Hepatic encephalopathy after transjugular intrahepatic portosystemic shunts: incidence and risk factors.
Am J Gastroenterol 1995 Apr;90(4):549–555. PMID: 7717309.
[12] Bai M, Qi XS, Yang ZP, et al. TIPS improves liver transplantation-free survival in cirrhotic patients with refractory ascites: an updated meta-analysis. World J Gastroenterol 2014 Mar 14;20(10):2704–2714.
[13] Bureau C, Garcia Pagan JC, Layrargues GP, et al. Patency of stents covered with polytetra fluoroethylene in patients treated by transjugular intrahepatic portosystemic shunts: long-term results of a randomized multicentre study. Liver Int 2007 Aug;27(6):742–747.
[14] Riggio O, Angeloni S, Salvatori FM, et al. Incidence, natural history, and risk factors of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt with polytetrafluoroethylene-covered stent grafts. Am J Gastroenterol 2008 Nov;103(11):2738–2746.
[15] Sarwar A, Esparaz AM, Chakrala N, et al. Efficacy of TIPS reduction for refractory hepatic encephalopathy, right heart failure, and liver dysfunction. AJR Am J Roentgenol 2021 May;216(5):1267–1272.
[16] Nardelli S, Bellafante D, Ridola L, et al. Prevention of post-tips hepatic encephalopathy: the search of the ideal candidate. Metab Brain Dis 2022 Nov 29.
[17] Nardelli S, Gioia S, Pasquale C, et al. Cognitive impairment predicts the occurrence of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt. Am J Gastroenterol 2016 Apr;111(4):523–528.
[18] Nardelli S, Lattanzi B, Torrisi S, et al. Sarcopenia is risk factor for development of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt placement. Clin Gastroenterol Hepatol 2017 Jun;15(6):934–936.
[19] Nardelli S, Lattanzi B, Merli M, et al. Muscle alterations are associated with
minimal and overt hepatic encephalopathy in patients with liver cirrhosis.
Hepatology 2019 Nov;70(5):1704–1713.
[20] Casado M, Bosch J, García-Pagán JC, et al. Clinical events after transjugular
intrahepatic portosystemic shunt: correlation with hemodynamic findings. Gastroenterology 1998 Jun;114(6):1296–1303.
[21] Schepis F, Vizzutti F, Garcia-Tsao G, et al. Under-dilated TIPS associate with efficacy and reduced encephalopathy in a prospective, non-randomized study of patients with cirrhosis. Clin Gastroenterol Hepatol 2018 Jul;16(7):1153–1162.e7.
[22] Praktiknjo M, Abu-Omar J, Chang J, et al. Controlled underdilation using novel
VIATORR? controlled expansion stents improves survival after transjugular
intrahepatic portosystemic shunt implantation. JHEP Rep 2021 Mar 3;3(3): 100264.
[23] Riggio O, Masini A, Efrati C, et al. Pharmacological prophylaxis of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt: a randomized controlled study. J Hepatol 2005;42:674–679.
[24] Bureau C, Thabut D, Jezequel C, et al. The use of rifaximin in the prevention of overt hepatic encephalopathy after transjugular intrahepatic portosystemic shunt : a randomized controlled trial. Ann Intern Med 2021 May;174(5):633–640.
[25] Cordoba J, Ventura-Cots M, Simón-Talero M, et al., CANONIC Study Investigators of EASL-CLIF Consortium. Characteristics, risk factors, and mortality of cirrhotic patients hospitalized for hepatic encephalopathy with and without acute-on-chronic liver failure (ACLF). J Hepatol 2014 Feb;60(2):275–281.
[26] Lucidi C, Ginanni Corradini S, Abraldes JG, et al. Hepatic encephalopathy expands the predictivity of model for end-stage liver disease in liver transplant setting: evidence by means of 2 independent cohorts. Liver Transpl 2016 Oct;22(10):1333–1342.
[27] Malinchoc M, Kamath PS, Gordon FD, et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 2000;31:864–871.
[28] Kamath PS, Kim WR. Advanced liver disease study group. The model for end-stage liver disease (MELD). Hepatology 2007;45:797–805.
[29] Bettinger D, Sturm L, Pfaff L, et al. Refining prediction of survival after TIPS with the novel Freiburg index of post-TIPS survival. J Hepatol 2021;74:1362–1372.
[30] Vizzutti F, Celsa C, Calvaruso V, et al. Mortality after transjugular intrahepatic portosystemic shunt in older adult patients with cirrhosis: a validated prediction model. Hepatology 2023 Feb 1;77(2):476–488.
[31] Mamiya Y, Kanazawa H, Kimura Y, et al. Hepatic encephalopathy after transjugular intrahepatic portosystemic shunt. Hepatol Res 2004 Nov;30(3):162–168.
[32] Nardelli S, Riggio O, Marra F, et al. Episodic overt hepatic encephalopathy after transjugular intrahepatic portosystemic shunt does not increase mortality in patients with cirrhosis. J Hepatol. 2024 Apr;80(4):596-602.
[33] Hartl L, Kornfehl A, Reiberger T. Does encephalopathy with early onset after TIPS impact on mortality? J Hepatol. 2024 Jun 3:S0168-8278(24)00421-5. Epub ahead of print.
(来源:《国际肝病》编辑部)
声明:本文仅供医疗卫生专业人士了解最新医药资讯参考使用,不代表本平台观点。该信息不能以任何方式取代专业的医疗指导,也不应被视为诊疗建议,如果该信息被用于资讯以外的目的,本站及作者不承担相关责任。
标签:
快讯
图片新闻
肝硬化
发表评论
全部评论
